When You Have Gastrointestinal (GI) Bleeding
Blood in your vomit or stool can be a sign of gastrointestinal (GI) bleeding. GI bleeding can be scary. But the cause may not be serious. You should always see your healthcare provider if you have GI bleeding.
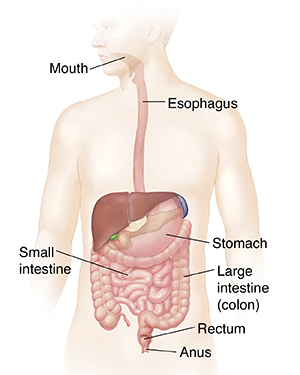
The GI tract is the path through which food travels in the body. Food passes from the mouth down the esophagus. This is the tube from the mouth to the stomach. Food starts to break down in the stomach. It then moves through the duodenum, the first part of the small intestine. Nutrients are absorbed as food travels through the small intestine. What is left passes into the colon (large intestine) as waste. The colon removes water from the waste. Waste continues from the colon to the rectum (where stool is stored). Waste then leaves the body through the anus. The upper GI tract is from the mouth through the duodenum. The lower GI tract is from the end of the duodenum to the anus.
Causes of GI bleeding
GI bleeding can be caused by many different problems. Some of the more common causes include:
-
Swollen veins in the anus (hemorrhoids)
-
Swollen veins in the esophagus (varices)
-
Sores (ulcers) on the lining of the GI tract
-
Cuts or scrapes in the mouth or throat
-
Infection caused by germs such as bacteria or parasites
-
Food allergies, such as milk allergy in young children
-
Medicines, especially aspirin, blood thinners, and NSAIDs (non-steroidal anti-inflammatory drugs) such as ibuprofen
-
Inflammation of the GI tract (gastritis or esophagitis)
-
Colitis (Crohn's disease or ulcerative colitis)
-
Cancer (tumors or polyps)
-
Abnormal pouches in the colon (diverticula)
-
Tears in the esophagus or anus
-
Nosebleed
-
Abnormal blood vessels in the GI tract (angiodysplasia)
Diagnosing the cause of blood in stool
If blood is coming out in your stool, you may have a lower GI tract problem or a very fast upper GI tract bleed. Bleeding from the GI tract can be bright red. Or it may look dark and tarry. Tests may also find blood in your stool that can’t be seen with the eye (occult blood). To find out the cause, tests that may be ordered include:
-
Blood tests. A blood sample is taken and sent to a lab for exam.
-
Hemoccult test. Checks a stool sample for blood.
-
Stool culture and other stool-based tests. These check a stool sample for bacteria or parasites, inflammation, and other problems.
-
X-ray, ultrasound, nuclear scan, or CT scan. Imaging tests that take pictures of the digestive tract.
-
Colonoscopy or sigmoidoscopy. This test uses a flexible tube with a tiny camera. The tube is inserted through your anus into your rectum to see the inside of your colon. Your healthcare provider can also take a tiny tissue sample (biopsy) to be looked at in a lab. They can also treat a bleeding source.
-
Capsule endoscopy. This test uses a tiny camera that is swallowed, passes through the intestine, and takes pictures of the small intestine. This is harder to reach with scopes.
Diagnosing the cause of blood in vomit
If you are vomiting blood or something that looks like coffee grounds, you may have an upper GI tract problem. To find the cause, tests that may be done include:
-
Upper endoscopy. A flexible tube with a tiny camera is inserted through your mouth and throat to see inside your upper GI tract. This lets your healthcare provider take a tiny tissue sample (biopsy) to be looked at in a lab. They can also treat a bleeding source.
-
Nasogastric lavage and aspiration. The provider may withdraw some of the fluid in the stomach to test it for bleeding. This can sometimes tell if you have upper GI or lower GI bleeding.
-
X-ray, ultrasound, nuclear scan, or CT scan. Imaging tests that take pictures of your digestive tract.
-
Upper GI series. X-rays of the upper part of your GI tract that are taken after you swallow a contrast drink.
-
Enteroscopy. This sends a flexible tube or a small, swallowed capsule camera into your small intestine.
Call 911
Call 911 if any of these occur:
When to call your healthcare provider
Call your healthcare provider right away if you have any of the following:
-
Fever of 100.4° F ( 38.0°) C or above, or as advised by your provider
-
Signs of fluid loss (dehydration). These include a dry, sticky mouth, decreased urine output, and very dark urine.
-
Belly (abdominal) pain